This is a syndicated post that first appeared at http://www.medizinethnologie.net/tibetan-formulas-workshop/
This three-day workshop (May 8-10, 2015) at EASTmedicine, University of Westminster, London brought together international expert physicians and scholars of Tibetan medicine – medical anthropologists, historians, ethno- and medical botanists, pharmacologists – working with and/or on Tibetan medicine, and also experts in Chinese medicine as well as IT specialists. Organised by Mona Schrempf, the author of this report, the workshop was funded by the British Academy/Small Leverhulme Research Grant, the Sino-British Fellowship Trust and IASTAM (International Association for the Study of Traditional Asian Medicine). It had the aim to discuss and contribute to what an interdisciplinary and multilingual digital knowledge base should look like that could be used in the future as a tool for documenting and analysing Tibetan medical formulas for a variety of scholarly users worldwide, including physicians of Tibetan medicine working in many different national contexts in Asia and the West.
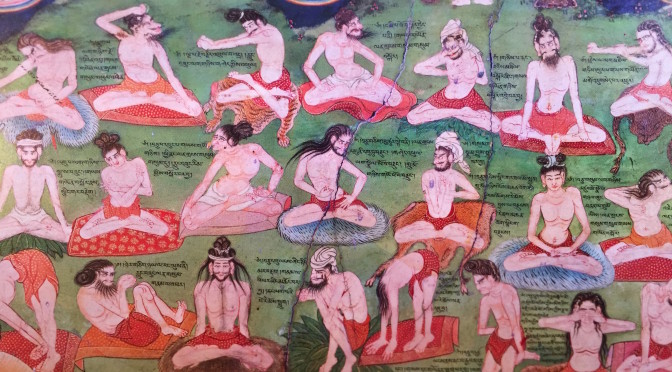
Such an ambitious endeavour requires complex processes of re-translation and re-contextualisation of and between Tibetan medicine and biomedicine (and partly Chinese medicine) in the relevant languages Tibetan, English, Latin, and Chinese, and also between different disciplines involved. Therefore, we focused on a common global ailment of our time that many of us universally suffer from – stress. We approached the topic from different angles, starting with a set choice of multicompound Tibetan formulas containing as main ingredient eaglewood. They are prescribed for specific types of ‘wind’ (Tib. rlung)[1] disorders in Tibetan medicine that are characterised by common stress symptoms – insomnia, restlessness, lack of concentration, light depression. ‘Wind’ is the principle of movement within the body and governs the functions of thought, breathing, and other physical movements, such as bowel movement, etc. in Tibetan medicine. Stress-related ‘wind’ disorders are usually caused by and located in or around the heart, i.e. by an imbalance of the ‘heart wind’ (Tib. snying rlung) or the ‘life-sustaining wind’ (Tib. srog ’dzin rlung).
Such ‘wind’ disorders are generally treated – next to using other treatment methods (nutrition, behaviour, massage, moxibustion) – with a specific set of Tibetan formulas containing as main ingredient eaglewood or agar wood (Lat. different types of Aquilaria; Tib. a ga ru or a gar)[2], in the following shortly called Agar-formulas (Agar 8, Agar 15, Agar 20, Agar 35, Sogdzin 11). Eaglewood is both a potent medicinal and fragrant resinous wood, also used in medicinal incense against insomnia (Agar 31). Its use is problematic because of the unresolved botanical identification of Aquilaria malaccensis that is endangered and CITES-listed[3]. Nevertheless, Agar-formulas are very popular and frequently prescribed in Tibetan medicine. They are produced and prescribed as compounded formulas by physician-cum-pharmacists or by physicians administering readily manufactured pills; however, they might be also directly taken as a dietary supplement.
We looked at different Agar-recipes and their various formulations, their ingredients and indications. At the workshop, Tibetan scholars also presented classical Tibetan medical texts and certain pharmacopoeias used for producing these formulas. It quickly became evident, however, that both the complexity of different disease categories and understandings of causes of illness in Tibetan medicine are not easily translatable into European biomedical or even ‘alternative medical’ understandings. On the other hand, it is possible and practiced already. Researchers at one pharmaceutical company in Europe producing Padma Nervetonic based on the Tibetan formula Sogdzin 11 explained at the workshop how and why they had to adapt or omit certain ingredients of the original formula which is administered for stress to European patients, how its overall efficacy is maintained and understood, as well as proven and regulated within European frameworks of production and distribution (on such a process of translation, see Schwabl and Vennos 2015).
Processes of cultural translation are intrinsic to correlating and making sense of illness and treatment between different languages, of medico-cultural concepts of health and disease, and of various disciplinary approaches and interests, yet they are vexed and problematic and therefore often ignored or glossed over. We tried to do the opposite in this workshop by carefully translating together the same formulas from different disciplinary perspectives and retranslating ‘in-between’ those. Prepared by a one-month pilot study by visiting scholar-physician of Tibetan medicine, Dr Cairang Nanjia from the Tibetan Medical College, Qinghai University, PRC, and the author of this report, Mona Schrempf – at the time Wellcome Trust Research Fellow at EASTmedicine, University of Westminster (2012-2015) – this ensuing workshop proved a fruitful platform for discussing some of the outcomes and issues involved. It is hoped that the initial results from this workshop will serve as a basis for future international research cooperations on the topic of Tibetan materia medica and formulae (Schrempf forthcoming a,b).
Our pilot-study examined Agar-formulas based on their original recipe texts and documentations as well as different application contexts in China and Europe. From a Tibetan medical point of view, it is impossible to narrow down the efficacy of a particular formula or even of a single ingredient within a formula to one specific disease only (usually defined in biomedical terms). Rather than perceiving this gap in translation between different medical principles as a loss, it can also open up a space for research examining how careful correlations between different medical principles can allow for a more complex and complete view of disease in relation to a particular formula, and maybe even shed light on possible causes and explanations on how disease can originate. Tibetan formulae are conceptualised in a way that they balance internally the different efficacies of single ingredients as to avoid side-effects while multitargeting connected imbalances in the body.
Traditionally, Tibetan formulae are not only prescribed for a particular imbalance in the body but individually according to the constitution of an individual patient and according to the stage of a disease or combination of disease(s), etc. For this subtle individual prescription, pulse diagnosis is necessary. It is the only way to know which particular imbalances are present or dominate and therefore in need of immediate treatment within a patient’s body. So how can this aetiological and epistemological complexity be translated into a fixed biomedical disease entity required to prove biomedically defined efficacy that is, for example, necessary for producing industrialised, quality approved and licensed pharmaceuticals? This is just one of the many questions of translation that we were addressing in this workshop[4].
The individual workshop presentations
Cairang Nanjia (Tib. Tsering Namgyal) began by documenting Agar-formulas in Tibetan medical, botanical and pharmacological texts used at present in Qinghai, China. He was focusing on the structure of the formulas, comparing the single ingredients and their relations to each other. We also looked at the different translations of these formulas into Chinese and English as well as German languages and prescription leaflets, adaptations that were sometimes also altering the actual composition of the formulas. The author of this report, Mona Schrempf, related her ethnographic material on different styles of production and prescription practices of Agar-formulas in both China and parts of Europe (Schrempf, in press, forthcoming a). With the advice from IT specialist Kapetanios, Cairang and Schrempf developed a possible multi-level digital knowledge base structure of synonyms and homonyms in order to deal with the complexity of different languages, concepts and terminologies connected with the Agar-formulas in an adequate way using different disciplinary approaches as access points to the digital knowledge base envisioned. The preliminary results were presented at the workshop for discussion and have benefitted, among others, specifically from the input by Bob Allkin, IT-specialist for digital Plant Names Services at the Royal Botanic Gardens Kew, London. He explained why plant names matter and how he organises Kew’s digital knowledge base using authoritative international naming and taxonomic resources, what the obstacles are for appropriate naming and use, how things can go wrong, and the role of the food and drug administration in deciding what is toxic and what not.
Workshop participants used different sources for looking at the Tibetan Agar-formulas and analysed them following up on specific questions, such as: Which texts are important for understanding Tibetan materia medica and formulas produced today? Who produces these formulas using what kind of knowledge and production technology, and how is this connected to (biomedically defined) efficacy and safety issues? Which ingredients are we actually talking about in a specific formula and how do we identify them botanically while addressing their regional diversity at the same time? How and why are certain materia medica ingredients in a formula substituted? How does a formula work and for what kind of disorders, related to which organs etc.? How can we understand ‘wind’ (Tib. rlung) disorders in Tibetan medicine correctly, and in particular, ‘heart wind’ and ‘life-sustaining wind’ treated by Agar-formulas? Is a translation between these specific wind-disorders and what we call ‘stress’ possible at all? Is it effective to prescribe an Agar-formula for stress symptoms without a prior detailed pulse diagnosis of the individual constitution of the patient and his or her specific disease by a physician of Tibetan medicine?
These are complex issues without doubt that we tried to address by re-translating between Tibetan, English and Chinese languages and inherent health and disease concepts in Tibetan and biomedicine as well as – at least where China is concerned – also in relation to Chinese medical concepts. The latter appear on package leaflets of Tibetan medicines in China, written in Chinese. Sources used and topics addressed at the workshop ranged from analysing Tibetan historical medical and botanical texts for developing a feasible structure for Tibetan formulas (Olaf Czaja) to Chinese publications on minority medicines and how information on their materia medica is collected in China (Lena Springer); how the seminal Tibetan medical text, the Four Tantras or rGyud bzhi explains the classification and treatment of rlungdisorders (Mingji Cuomu); how specific rlung disorders, specially ‘heart wind’ (Tib. snying rlung) and ‘life sustaining wind’ (Tib. srog ’dzin rlung), are taught to Tibetan medical students in Xining (Sanjijia); and what the experiences with treating rlung disorders at the Tibetan medical hospital in Xining are, demonstrated by the eminent 84 year old co-founder, teacher and physician-cum-pharmacist, Akhe Nyima.
Colin Millard presented patient case studies and related prescription practices by Lobsang Dhonden Soktsang for ‘wind’ disorders at the Tara Clinics, UK, in which, however, no Agar-compounds were used. IT-specialist Bob Allkin and medical botanist Christine Leon from the Royal Botanic Gardens Kew gave stunning presentations of the complexity of identifying just one single plant in a botanically correct way. In contrast, the ethno-botanist van der Valk asked questions on whether the fixation on a specific botanical identity of, for example, ‘eaglewood’, does not counteract or limit the diversity and regional flexibility of this particular medicinal plant.
This flexibility is also connected with the sustainability of these plants used in many Tibetan formulas whose ingredients mostly grow in the wild in the Himalayas and on the Tibetan Plateau – and are often locally not accessible for small scale producers, such as private physician-cum-pharmacists. Padma Gurmet from the Sowa Rigpa Institute in Ladakh demonstrated the ongoing efforts to cultivate and sustain medicinal plants growing in the wild in Ladkah. Brion Sweeney demonstrated the important work by the eminent scholar and teacher Akong Rinpoche in both his home area of Kham and the UK for Tibetan medicine focusing on the sustainability of medical plants and Tibetan medical education. Florian Ploberger discussed the Tibetan materia medica of Agar-formulas from the point of view of TCM-phytotherapy. Herbert Schwabl, director of research at Padma AG, and Cecile Vennos, head of regulatory and medical scientific affairs, explained how they had adapted the Tibetan formula Sogdzin 11 into becoming Padma Nervotonin (Schwabl & Vennos 2015). Last but not least, Michael Stanley-Baker, Chen Shi-Pei, and Brent Haoyang Ho from the Max Planck Institute for the History of Science, Berlin, explained what a digital data base can offer if one is interested in mapping drugs across time and space.
Perspectives
The aim of the workshop was to sound out what kind of information is important in order to fully document and analyse Tibetan medical formula in a multidisicplinary and multilingual digital knowledge base. Only careful translations will allow to properly correlate different concepts used and applied to these formulas, from Tibetan, Chinese and bio-medical knowledge, the impact of regulatory regimes on the formulas in each national context. It would be desirable if in the future we could pursue an integrative and synthesising approach to Tibetan Medicine with a sensitivity to various interpretations in this multi-lingual endeavour and one which adequately represents the varying involved disciplines and therapeutic practices. The aim would be to explore careful and meaningful ways of representing Tibetan cultural and medical knowledge and develop suitable key search terms in different semantic networks as to make such a digital knowledge base a useful tool for researchers and practitioners alike.
On the workshop, see the website of EASTmedicine, University of Westminster.
Footnotes
[1] ‘Wind’ or loong (rlung) in Tibetan is one of three complex bodily principles in Tibetan medicine, the other two being ‘bile’ or tripa (Tib. mkhris-pa) and ‘phlegm’ or peken (Tib. bad-mkan), resembling Ayurvedic principles with which they are historically connected. An imbalance of these three bodily principles causes disease. For more information, see http://tibet-medicine.org/de/tibetische-medizin/grundlagen/die-grundprinzipien/
[2] One of the problems we are facing is the botanical identification and regional variety of this plant. It can be, for example, Aquilaria agallocha Roxb., Aquilaria sinensis, Cinnamomum pharthenoxylon Tack.
[3] On the Convention on International Trade in Endangered Species of Wild Fauna and Flora (CITES), see https://cites.org/eng/disc/what.php. On Aquilaria mallacensis, see http://www.iucnredlist.org/details/32056/0
[4] Medical anthropological research publications on Tibetan medicine alias Sowa Rigpa (Tib. gso ba rig pa), the ‚Science of Healing‘, mainly as practiced in Asia, are growing. See Adams, Schrempf & Craig 2010; Blakie 2013, 2015; Craig 2012; Janes 2002; Hofer 2012; Kloos 2013; Pordié 2008; Saxer 2013, Schrempf 2007, in press, forthcoming a,b.
References
Adams, Vincanne, Mona Schrempf & Sienna Craig (Hgs). 2010 (2013). Medicine Between Science and Religion – Explorations on Tibetan Grounds. London, New York: Berghahn Publishers.
Blakie, Calum. 2013. Currents of Tradition in Tibetan Medicine Pharmacy. In: East Asian Science, Technology and Society 7 (3), 425-451.
—— 2015. Wish-fulfilling Jewel Pills: Tibetan Medicines from Exclusivity to Ubiquity. In: Anthropology and Medicine22 (1), 7-22. DOI: 10.1080/13648470.2015.1004504
Craig, Sienna. 2012. Healing Elements: Efficacy and the Social Ecologies of Tibetan Medicine. Berkeley: University of California Press.
Janes, Craig. 2002. Buddhism, Science, and the Market: The Globalisation of Tibetan Medicine. In: Anthropology and Medicine 9 (3), 267-289.
Hofer, Theresia. 2012. The Inheritance of Change. Transmission and Practice of Tibetan Medicine in Ngamring. Wien: Arbeitskreis für Tibetische Buddhistische Studien Universität Wien, Wiener Studien zur Tibetologie und Buddhismuskunde, Heft 76.
Kloos, Stephan. 2013. How Tibetan medicine in Exile Became a „Medical System“. In: East Asian Science, Technology and Society 7 (3), 381-395.
Pordié, Laurent (Hg). 2008. Tibetan Medicine in the Contemporary World. Global Politics of Medical Knowledge and Practice. London & New York: Routledge.
Saxer, Martin. 2013. Manufacturing Tibetan Medicine. The Creation of an Industry and the Moral Economy of Tibetanness. Oxford, New York: Berghahn Publishers.
Schrempf, Mona. 2007. Soundings in Tibetan Medicine. Historical and Anthropological Perspectives (Proceedings of the 10th Seminar of the International Association for Tibetan Studies (PIATS), Oxford 2003). Leiden: Brill Academic Publishers.
—— (2015, in press). ‘Formulation Regimes and Styles of Practice in Transnational Tibetan Medicine – a Comparative Perspective on Efficacy and Safety between China and Europe. In: Mona Schrempf & Lena Springer (Hgs). Efficacy and Safety in Tibetan and Chinese Medicine: Historical and Ethnographic Perspectives (special issue) Asian Medicine – Tradition and Modernity 10 (1-2), 35 p.
——(forthcoming a) A Tibetan Medical Root Formula and its Derivatives: Cultural Translations in Transnational Styles of Practice.
——(forthcoming b) Transnational Tibetan Medicine – Formula Regimes, Therapeutic Networks and Styles of Practice between China and Europe (Berghahn Publishers)
Schwabl, Herbert & Cecile Vennos. 2015. From Medical Tradition to Traditional Medicine: A Tibetan Formula in the European Framework. In: Journal of Ethnopharmacology 167 (5), 108-114.